NHS Services
- Home
- NHS Services
First Contact Physiotherapy services
With the NHS Long Term Plan and the new GMS contract to employ more than 20,000 healthcare professionals as part of the wider primary care multidisciplinary team. First contact MSK practitioners (FCP) are a vital element of this new workforce.
A well run FCP model could assist GP’s by reducing the number of GP led appointments required, freeing up capacity for other duties and types of appointments. It also has the additional benefits of improving the practices MSK knowledge, streamlining the MSK pathway with improved referral to secondary care and higher surgery conversion rates.
This means that a patient presenting to a GP practice with an MSK condition can see a FCP at their first appointment, accelerating their MSK assessment, treatment plan and (if appropriate) investigations and referral, along with saving both time and resources within primary care teams.
As regulated MSK practitioners, FCPs work at an Advanced Clinical Practice (ACP) level. This “is a level of practice characterised by a high degree of autonomy and complex decision making… It includes the analysis and synthesis of complex problems across a range of settings, enabling innovative solutions to enhance people’s experience and improve outcomes”. 1 The skills and knowledge required for this role are attained through postgraduate-level MSK learning, which may include independent prescribing skills, injection therapy skills.
A review of recent and ongoing FCP pilots demonstrates:
- Quicker recovery for patients with 50-70% discharged after one consultation
- Integration of Shared Decision Making early into a patient’s pathway
- Improved use of diagnostic capacity with 3-5% cost reductions in plain X-rays and MRI scans ordered from general practice
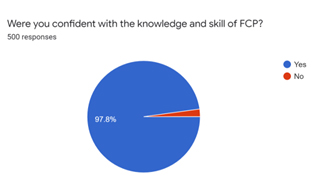
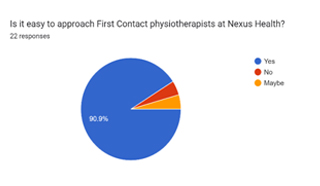
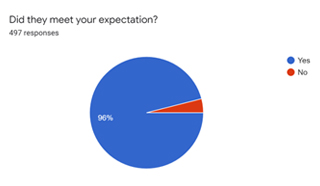
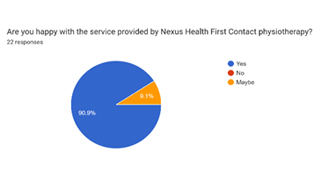
- More appropriate referrals to secondary care (improved conversion rates for orthopaedic surgery 80- 99%) Good patient experience with 90-99% satisfaction rates.
Please see the recent survey done in December 2022
Primary Care Networks and/or Federations could choose to employ the first contact practitioners themselves; however, this also means taking on the training needs for what in all but the largest PCN’s would be a single clinician, whose practice and supervision needs the PCN may be unfamiliar with.
It would also involve arranging rota’s, holiday and long term sick cover, potentially dealing with lone working or an isolated individual that could lead to deskilling of the clinician and a reduction in the value of the FCP. The PCN would also need to provide the equipment required, deal with pay and pensions, most likely under agenda for change terms, ensure the insurance for the clinicians and practice is adequate and deal with any HR issues that arise.
With a contractor model none of these problems are the PCN’s, and as the commissioner you get to decide what issues are of most importance to your area and work with the provider to ensure these are the services highest priority.
Why Nexus Health?
Nexus Health Limited is run by clinicians with over 10 years’ experience in running MSK services in private and public sectors. Nexus Health is already providing FCP service to 10 PCNs in Hertfordshire, Reading and Nottingham.
From a FCP perspective we have strict criteria that all FCP’s should have passed defined competency training for deployment into the primary care setting. Further gains can be made with gradual deployment of advanced clinicians with extended skills such as Independent Prescribing, Injection therapy, or postgraduate training in the management of patients with chronic pain.
Overall, the majority of gains for embedding FCP’s into primary care in terms of reducing GP’s appointments, improving patient access, patient care and healthcare outcomes are best demonstrated with placement of clinicians with extended skill sets and working to the ceiling of their professional licence.
The experience and quality of our clinicians means we are also able to demonstrate an excellent patient safety record, assessing and recording red flags, informed consent, subjective and objective patient history and the effective management of non-MSK conditions that have been identified through a broader co- morbidity knowledge.
FCP Service implementation
For the service to be effective and for the local GP’s to see an improvement in their workload with investment of the likely DES funding we would look to provide one session of FCP for every 5000 registered patients each week. These sessions would be distributed to each of the practices within the PCN’s so that all surgeries feel the benefit relative to their list size.
The service would be supported by an operational manager overseeing its delivery and management Alongside the operational manager would be a clinical team lead, who may work in the service day to day but would also have time set aside to take ownership for the clinical effectiveness and safety of the service by reviewing audits, supervising the team, providing training etc.
For the service to be fully integrated with the PCN we would suggest the team to work on the existing GP PAS unit, with access given to the services operations manager to be able to oversee the work done and report back to the GP’s and internally on the work the team are doing. We would also naturally expect the administration support to come from the local GP surgeries so they could book directly into the clinics, ensuring that the correct patients are booked in to the FCP clinics.

